Is MCAS Genetic? Unraveling The Mystery Behind Mast Cell Activation Syndrome
Ever wondered if MCAS is genetic? If you're here, chances are you're either dealing with this condition or know someone who is. Mast Cell Activation Syndrome (MCAS) has been a topic of growing interest in recent years, and for good reason. It's a complex condition that affects how your body responds to allergens, infections, and even stress. But is it something you’re born with, or does it develop over time? Let’s dive in and find out!
MCAS isn't your run-of-the-mill health issue. Unlike a cold or flu, it affects the way your mast cells behave. These cells are like the security guards of your immune system, but in people with MCAS, they tend to overreact, releasing too many chemicals and causing all sorts of symptoms. And here’s the kicker—scientists are still figuring out exactly why this happens.
So, is MCAS genetic? That's the million-dollar question we're here to answer. Stick around, and we’ll break it down step by step. By the end of this article, you’ll have a clearer understanding of the genetic factors behind MCAS and how it impacts your life. Let’s get started!
- Tony Vitello Is He Married Unraveling The Personal Life Of The Esteemed Coach
- Discovering The Age Of Bill Belichicks Wife
Here’s a quick rundown of what we’ll cover:
- What is MCAS?
- Is MCAS Genetic?
- Common Symptoms of MCAS
- How is MCAS Diagnosed?
- Treatment Options for MCAS
- Genetic Testing for MCAS
- Lifestyle Changes for Managing MCAS
- Current Research on MCAS Genetics
- Can MCAS Be Prevented?
- Wrapping It Up
What is MCAS?
MCAS stands for Mast Cell Activation Syndrome, and it’s essentially a condition where your mast cells—those little guys in your immune system—go into overdrive. Normally, mast cells release chemicals like histamine to protect your body from threats. But in MCAS, they release way too much, leading to a whole host of symptoms.
Think of mast cells as the bouncers at a club. When everything's cool, they let the good stuff in and keep the bad stuff out. But if they start overreacting, they might kick out innocent people or let in troublemakers. That’s kinda what happens in MCAS.
- Unlocking The Mystery Discovering What Page Does My Site Rank On Google
- Discover Your Online Presence See Where Your Website Ranks
MCAS can affect anyone, regardless of age or gender. And while it’s not as common as, say, allergies, it’s definitely something that’s gaining more attention in the medical world. But here’s the thing—scientists are still trying to figure out exactly what causes it, and whether genetics play a role.
Is MCAS Genetic?
Unpacking the Genetic Component
Now, let’s talk about the big question: Is MCAS genetic? The answer is… it’s complicated. While there’s no definitive proof that MCAS is entirely genetic, there’s definitely evidence suggesting that genetics can play a role.
Research has shown that some people with MCAS have mutations in specific genes that control mast cell behavior. These mutations can make mast cells more likely to overreact, leading to the symptoms of MCAS. But here’s the thing—just because you have these mutations doesn’t mean you’ll definitely develop MCAS. Other factors, like environmental triggers, also come into play.
So, while genetics might increase your risk, it’s not the only factor. Think of it like this: genetics loads the gun, but environment pulls the trigger.
Common Symptoms of MCAS
MCAS can cause a wide range of symptoms, and they often vary from person to person. Some folks might experience mild symptoms, while others could be dealing with something more severe. Here’s a quick rundown of the most common ones:
- Itchy skin or hives
- Swelling (especially in the face or hands)
- Gastrointestinal issues like bloating or diarrhea
- Shortness of breath or wheezing
- Headaches or migraines
- Fatigue or brain fog
See what I mean? MCAS can really mess with your body in all sorts of ways. And because the symptoms are so varied, it can be tough to diagnose. But don’t worry—we’ll get into that next.
How is MCAS Diagnosed?
Testing for MCAS
Diagnosing MCAS isn’t as simple as running a blood test or taking an X-ray. Doctors usually rely on a combination of tests and observations to figure out if someone has MCAS. Here are some of the most common methods:
- Histamine levels: Doctors might check your blood or urine for elevated levels of histamine, which is one of the chemicals mast cells release.
- Tryptase levels: Tryptase is another chemical released by mast cells, and high levels can indicate MCAS.
- Clinical symptoms: Your doctor will also look at your symptoms and medical history to see if they match up with MCAS.
It’s worth noting that diagnosing MCAS can be tricky, especially since its symptoms overlap with other conditions. That’s why it’s so important to work with a knowledgeable healthcare provider who’s familiar with MCAS.
Treatment Options for MCAS
Once you’ve been diagnosed with MCAS, the next step is figuring out how to manage it. While there’s no cure for MCAS, there are plenty of treatment options that can help you feel better. Here are some of the most common ones:
- Antihistamines: These meds can help control symptoms like itching and hives.
- Leukotriene inhibitors: These block the action of leukotrienes, which are chemicals involved in inflammation.
- Corticosteroids: These can reduce inflammation and swelling, but they’re usually only used for short-term relief.
Besides medication, lifestyle changes can also make a big difference. We’ll talk more about that later, but for now, just know that managing stress, avoiding triggers, and eating a healthy diet can all help keep MCAS symptoms in check.
Genetic Testing for MCAS
Is It Worth It?
Genetic testing is becoming more and more popular, and for good reason. It can give you valuable insights into your health risks and help you make informed decisions about your care. But when it comes to MCAS, is genetic testing really worth it?
The short answer is… maybe. While there are specific genetic mutations associated with MCAS, they’re not the only factor. Plus, genetic testing can be expensive, and it might not always provide clear answers. That said, if you have a family history of MCAS or other immune-related conditions, it could be worth discussing with your doctor.
Just remember—genetic testing is a tool, not a magic bullet. It can provide useful information, but it’s not the only thing you should rely on.
Lifestyle Changes for Managing MCAS
When it comes to managing MCAS, lifestyle changes can be just as important as medication. Here are a few tips to help you keep your symptoms under control:
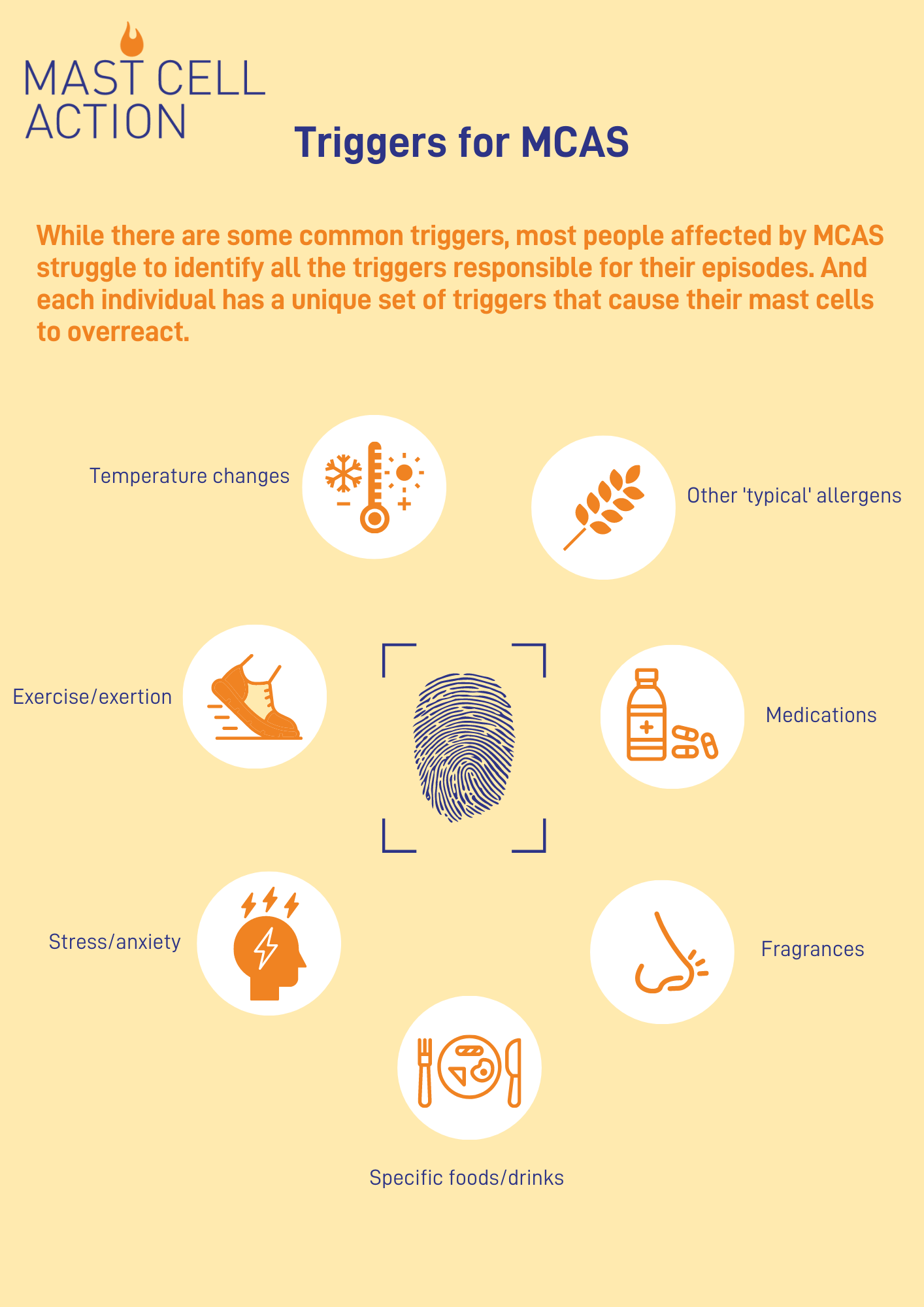
- Identify and avoid triggers: Common triggers include certain foods, medications, and even stress. Keep a journal to track what sets off your symptoms.
- Eat an anti-inflammatory diet: Focus on whole, unprocessed foods like fruits, veggies, lean proteins, and healthy fats.
- Practice stress management: Techniques like meditation, yoga, or deep breathing can help reduce stress and its impact on your symptoms.
Remember, everyone’s different, so what works for one person might not work for another. It’s all about finding what works best for you.
Current Research on MCAS Genetics
Scientists are constantly learning more about MCAS and its genetic components. Recent studies have identified several genes that may play a role in the development of MCAS, including ones involved in mast cell signaling and regulation. But there’s still a lot we don’t know.
One promising area of research involves looking at epigenetics, which is the study of how environmental factors can affect gene expression. This could help explain why some people with genetic predispositions develop MCAS while others don’t.
As research continues, we’ll likely gain a better understanding of the genetic and environmental factors that contribute to MCAS. And that could lead to more effective treatments down the road.
Can MCAS Be Prevented?
Here’s the thing—since we don’t fully understand what causes MCAS, it’s hard to say whether it can be prevented. But there are definitely steps you can take to reduce your risk:
- Stay healthy: Eating a balanced diet, exercising regularly, and getting enough sleep can help support your immune system.
- Avoid triggers: If you know certain things set off your symptoms, try to avoid them as much as possible.
- Manage stress: Chronic stress can weaken your immune system, so finding ways to manage it is key.
While these steps might not completely prevent MCAS, they can definitely help reduce your risk and improve your overall health.
Wrapping It Up
So, is MCAS genetic? The answer is a bit complicated. While genetics can definitely play a role, they’re not the only factor. Environmental triggers, lifestyle choices, and even stress can all contribute to the development of MCAS.
If you’re dealing with MCAS, remember that you’re not alone. There are plenty of treatment options available, and making lifestyle changes can make a big difference. And as research continues, we’ll likely gain a better understanding of this condition and how to manage it.
Before I go, I wanna leave you with one last thought: Knowledge is power. The more you know about MCAS and its genetic components, the better equipped you’ll be to take control of your health. So keep learning, keep asking questions, and don’t be afraid to advocate for yourself.
And hey, if you found this article helpful, drop a comment below or share it with someone who might benefit from it. Let’s spread the word about MCAS and help others understand this complex condition. Thanks for reading, and take care!
- Unlocking Your Websites Visibility How To Check Your Website Ranking In Google
- Mastering Your Online Presence With An Seo Ranking Checker For Google

MCAS Select.麥格格物 Hong Kong Hong Kong
MCAS triggers Mast Cell Action

2025 MCAS Beaufort Airshow